Introduction
Fibrin hydrogels are protein-based scaffolds frequently used in tissue engineering for delivery of bioactive payloads (e.g., growth factors). Conventional fibrin scaffolds enable very limited spatial and temporal control of payload release, especially after implantation. This is potentially problematic because tissue regeneration is tightly regulated by biomolecules in a spatiotemporal manner.1 We have designed acoustically responsive scaffolds (ARSs) that will enable on-demand, spatiotemporally controlled payload release from a hydrogel scaffold using focused ultrasound (US) as the triggering mechanism. ARSs are formed by incorporating sonosensitive perfluorocarbon (PFC) double emulsions into the fibrin hydrogels. Sonosensitive PFC emulsions are used because of their biocompatibility, inertness, and acoustic sensitivity. Water-soluble payloads are contained within the W1 phase, and each interface (i.e., W1 /PFC and PFC/W2 ) is stabilized by a nonionic surfactant. Control of payload release from the ARS is achieved using nonthermal US, termed acoustic droplet vaporization (ADV), whereby the PFC phase within the emulsion vaporizes when exposed to US above an acoustic threshold.2,3 ADV is triggered using focused, megahertz frequency US, which means submillimeter precision is obtainable, even within deep tissue. Most importantly, the use of US to modulate ARSs enables noninvasive controlled release of the encapsulated payload after the scaffold has been implanted.
Methods
Emulsion Preparation. Sonosensitive double emulsions, with the structure water-in-PFC-in-water (W1 /PFC/W2 , mean diameter: 2.1 ± 0.1 µm), were prepared following a previous method.4 Briefly, a triblock fluorosurfactant, consisting of Krytox synthetic oil and polyethylene glycol (molecular weight [MW]: 1 kDa) was dissolved in 1 g of PFC at 2% (w/w). The PFC phase consisted of perfluorohexane (C6, C6 F14, 56°C boiling point) or a 1:1 admixture of perfluorohexane and perfluoropentane (C5, C5 F12, 29°C boiling point). The PFC solution was then combined, 2:1 (v/v), with an aqueous solution of Alexa Fluor 680-labeled dextran (AF680, MW: 10 kDa) reconstituted at 0.625 mg/mL in Dulbecco’s phosphate-buffered saline (DPBS). This concentration of dextran was chosen to prevent self-quenching of the fluorophore. The phases were sonicated for 30 s while on ice. The resulting primary emulsion, with a water-in-PFC (W1 /PFC) structure, was added dropwise to a solution of 50 mg/mL of Pluronic F68 nonionic surfactant in DPBS and stirred at 700 rpm for 2 min while on ice. The particle size of the resulting coarse double emulsion (W1 /PFC/W2 ) was reduced using a homogenizer at 29,900 rpm.
ARS Fabrication. ARSs were prepared using 10 mg/mL of clottable protein by first combining bovine fibrinogen dissolved in degassed (36% O2 saturation) Dulbecco’s modified Eagle’s medium (DMEM), with bovine thrombin (20 U/mL), 0.025 U/mL of aprotinin, and 1% (v/v) emulsion. ARSs containing emulsion with either the PFC admixture (i.e., C5/C6) or C6 are referred to as C5/C6-ARS and C6-ARS, respectively.
In Vitro Release Studies. For in vitro release studies, 0.5 mL of ARSs was cast in 24-well Bioflex plates and covered with 0.5 mL of DMEM. ARSs were exposed to focused US (2.5 MHz, peak rarefactional pressure = 8 MPa, 13 cycles, 100 Hz pulse repetition frequency) for 2 min daily (starting on day 1). To quantify the amount of AF680 released from the ARS, aliquots of the overlying media were sampled throughout the experiment and analyzed with a plate reader.
In Vivo Release Studies. This in vivo research was conducted with approval of the Institutional Animal Care and Use Committee at the University of Michigan. ARSs (0.25 mL volume per ARS) were prepared as described previously and injected subcutaneously in the lower back of BALB/c mice and polymerized in situ. After polymerization, subsets of the implanted ARSs were exposed to US (same parameters as previously described). Animals were imaged periodically using a preclinical fluorescence imaging system to quantify the dextran signal remaining in each implant.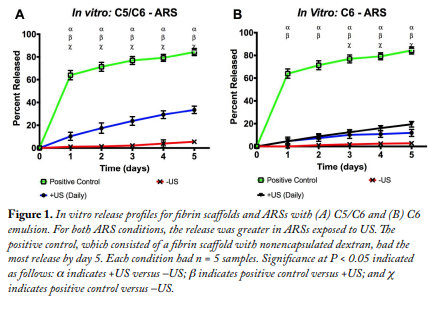
Statistics. All statistical analyses were performed with GraphPad Prism software. All data are expressed as the mean ± standard error of the mean of measured quantities. All n values are listed below each corresponding figure. Statistically significant differences were determined with a Student’s t test corrected for multiple comparisons using the Holm–Sidak method, with differences deemed significant for P < 0.05.
Results
AF680 was used as the model payload for all experiments because it can be easily quantified both in vitro and in vivo. Figure 1A shows that on day 5 C5/C6-ARSs exposed to US (i.e., +US) had 33.5 ± 3.3% payload released versus identical ARSs not exposed to US (i.e., –US, 5.5 ± 1.8%). The difference between +US and –US is evident on the initial day of US exposure, with 10.2 ± 1.6% released for +US and 1.2 ± 0.1% for –US. This trend follows for C6-ARSs (Fig. 1B), with 2.8 ± 0.3% released for –US and 19.4 ± 2.4% released for +US on day 5. Both data sets show statistically significant differences between +US and –US starting on day 1. The positive control, which was a conventional 10 mg/mL of fibrin hydrogel containing nonencapsulated AF680, had 84.4 ± 3.1% payload released by day 5.
In Figure 2, US caused release of the AF680 payload in the ARS, which was subcutaneously implanted in a mouse. The released payload was absorbed and eventually cleared by the subcutaneous vasculature.  The clearance caused a decrease in fluorescence signal, which was monitored noninvasively with a preclinical imaging system. In Figure 3, greater payload release was observed at day 7 for +US ARSs versus –US ARSs (C5/C6: –US, 67.8 ± 1.9% and +US, 89.3 ± 1.0% versus C6: –US, 51.7 ± 9.6% and +US, 85.9 ± 7.1%). Mice with C5/C6-ARSs and C6- ARSs showed statistically significant differences between +US and –US starting on day 1 and day 3, respectively.
The clearance caused a decrease in fluorescence signal, which was monitored noninvasively with a preclinical imaging system. In Figure 3, greater payload release was observed at day 7 for +US ARSs versus –US ARSs (C5/C6: –US, 67.8 ± 1.9% and +US, 89.3 ± 1.0% versus C6: –US, 51.7 ± 9.6% and +US, 85.9 ± 7.1%). Mice with C5/C6-ARSs and C6- ARSs showed statistically significant differences between +US and –US starting on day 1 and day 3, respectively.
Conclusions
Controlled release from an ARS can be achieved using focused US. Both in vitro (Fig. 1) and in vivo (Figs. 2 and 3) results show that greater dextran release is obtained with +US versus –US. When exposed to identical experimental conditions, C6- ARSs displayed lower nonselective (i.e., –US) and selective (i.e., +US) release compared with the C5/ C6-ARSs. This may be due to the greater stability provided by ARSs formulated from a higher boiling point PFC such as C6 (56°C) versus an admixture of C5 (29°C) and C6. Greater payload retention occurred in vitro with the –US condition compared with in vivo. In particular, Figure 3A shows that on day 1 a large fraction of the payload was released in the –US condition; however, the addition of US increased the release by more than 9% (absolute). This quick release of payload was not observed in C6-ARSs, which showed no differences between +US and –US until day 3. Future studies will be focused on understanding how various properties of the ARS impact release and applying this controlled delivery system for therapeutic angiogenesis.
Acknowledgements
This work was supported by National Institutes of Health (NIH) grant R21AR065010 (M. L. Fabiilli) and the Basic Radiological Sciences Innovative Research Award (M. L. Fabiilli). A. Moncion was supported by the National Science Foundation Graduate Student Research Fellowship (Grant No. DGE 1256260).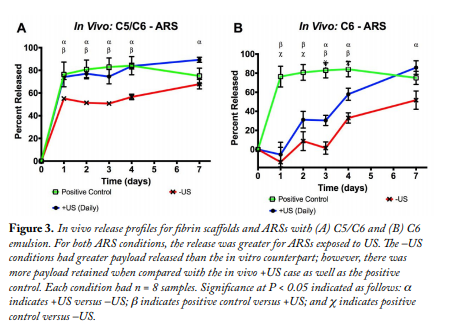
References 1. Richardson, TP, Peters, MC, Ennett, AB, Mooney, DJ. Polymeric system for dual growth factor delivery. Nature Biotechnol. 19: 1029-1034 (2001). 2. Moncion, A, Arlotta, KJ, Kripfgans, OD, Fowlkes, JB, Carson, PL, Putnam, AJ, Franceschi, RT, Fabiilli, ML. Design and characterization of fibrin-based acoustically responsive scaffolds for tissue engineering applications. Ultrasound Med. Biol. 42: 257-271 (2016). 3. Kripfgans, OD. Acoustic droplet vaporization for diagnostic and therapeutic applications. University of Michigan, Ann Arbor, MI (2002). 4. Fabiilli, ML, Wilson, CG, Padilla, F, Martin-Saavedra, FM, Fowlkes, JB, Franceschi, RT. Acoustic droplet–hydrogel composites for spatial and temporal control of growth factor delivery and scaffold stiffness. Acta Biomater. 9: 7399-7409 (2013).


